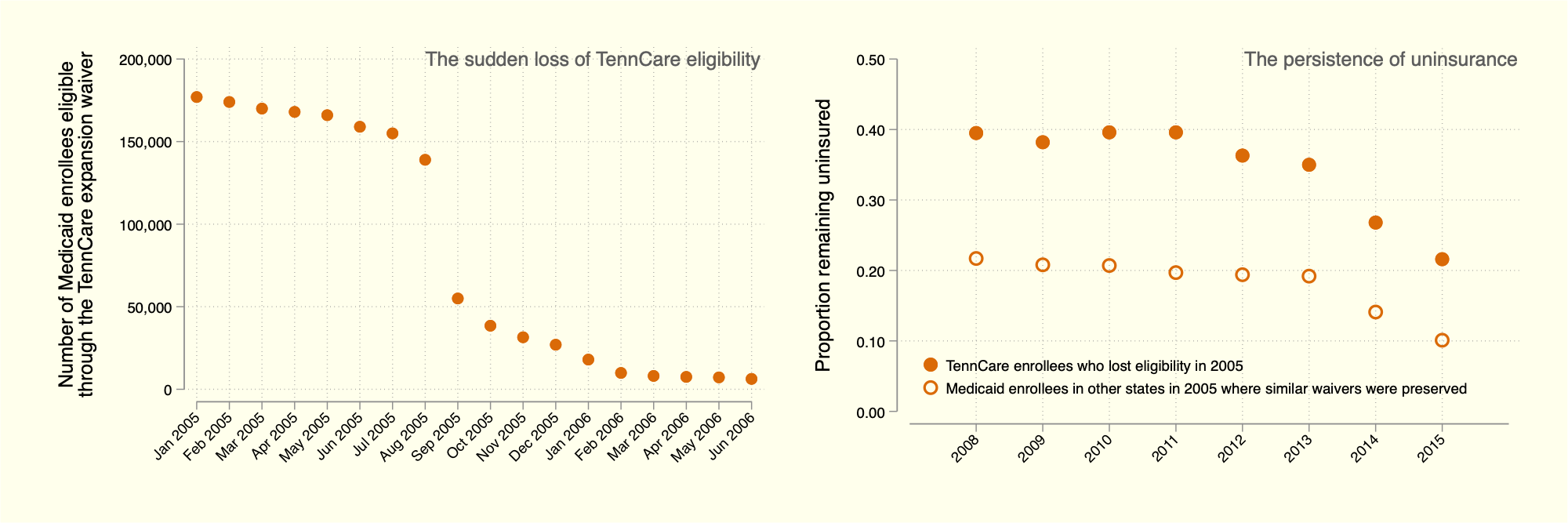
Above: We first illustrate the sudden cut to Medicaid eligibility among working-age adults in Tennessee in the middle of 2005. We then plot the fraction of (i) the “TennCare disenrollees” who remained uninsured many years after losing eligibility and (ii) adults enrolled in Medicaid in 2005 in states where similar waivers for eligibility remained intact.
Link to working paper
Abstract
Once considered a model for national health insurance reform, Tennessee’s Medicaid program, TennCare, later experienced one of the largest cuts to public health insurance in US history. The severe and sudden curtailing of Medicaid eligibility for a vulnerable population may have led to both short and long-term impacts to their health insurance, labor market, and health outcomes. Although the “TennCare disenrollment” has been studied in the past, never has the set of disenrollees been specified and tracked over a long period of time, as we do in this paper by linking administrative enrollment records from CMS to large household surveys from the Census Bureau. Our unique dataset allows us to pinpoint individuals who lost TennCare eligibility and trace their long-term outcomes. We first show that nearly half of the approximately 170,000 TennCare disenrollees were still uninsured several years after the disenrollment. Although many disenrollees obtained insurance through an employer, we do not find increases in labor force participation or employment among the disenrolled. We do find, however, evidence that employees increased hours worked, ostensibly to qualify for health insurance with their employer. Finally, we consider the health outcomes of the disenrollees, namely self-reported disability and mortality. This investigation yields mixed results. While disability shows a null result, we find statistically significant impacts on long-run mortality. Upon a more comprehensive analysis of public health insurance on mortality, however, we refrain from a determination, as our work warrants additional research into the relationship between public health insurance and health. Collectively, our results are largely consistent with the experimental literature but partially contrast with the quasi-experimental literature on the impacts of health insurance. Our findings come at a time when Medicaid faces budgetary challenges, and we conclude our paper by discussing several lessons from the TennCare experience that may inform current policy discussions. We also emphasize that our template can be applied to study other changes in access to Medicaid, such as the unwinding of pandemic provisions or large future Medicaid cuts, should they occur.
Disclaimer: Any views expressed are those of the authors and not those of the U.S. Census Bureau. The Census Bureau has reviewed this data product to ensure appropriate access, use, and disclosure avoidance protection of the confidential source data used to produce this product. This research was performed at a Federal Statistical Research Data Center under FSRDC Project Number 2603. (CBDRB-FY21-P2603-R09240, CBDRB-FY25-P2603-R11872/12193)